The exploration of TIM-3 Alzheimer’s treatment is paving the way for groundbreaking advances in combating Alzheimer’s disease. Recent studies indicate that turning off the TIM-3 checkpoint molecule could unleash the brain’s immune cells, known as microglia, to actively clear harmful plaques that impede cognitive function. This innovative approach draws on immune system therapy traditionally applied in cancer treatment, offering a new avenue for cognitive improvement in Alzheimer’s patients. Results from preclinical trials in mice have shown promising enhancements in memory performance, highlighting the potential for significant breakthroughs in treating this devastating condition. As research progresses, the implications of TIM-3 in restoring microglia function and ultimately improving quality of life for millions become increasingly evident.
The potential of TIM-3 in Alzheimer’s therapy represents a novel fusion of neurological science and immune modulation strategies. By investigating inhibitors that target the TIM-3 molecule, scientists aim to enhance microglial activity, which is crucial for the clearance of amyloid plaques associated with cognitive decline. This innovative concept aligns with broader cancer treatment strategies that harness the immune system to act against diseases. As breakthroughs in this domain unfold, they may redefine how medical professionals approach the management of Alzheimer’s disease, ultimately leading to improved outcomes for affected individuals. The growing intersection of immunology and neurodegenerative research opens exciting doors for future therapy developments.
Understanding the Role of TIM-3 in Alzheimer’s Treatment
TIM-3, or T cell immunoglobulin mucin-3, has emerged as a significant player in the landscape of Alzheimer’s research. Its expression on microglia, the brain’s resident immune cells, is particularly relevant in the context of Alzheimer’s disease (AD). In healthy individuals, microglia play a crucial role in clearing amyloid-beta plaques, which are hallmarks of Alzheimer’s pathology. However, when TIM-3 levels are elevated, these microglia become inhibited and are unable to effectively perform their clearing function. This blockade not only allows the accumulation of toxic plaques but also contributes to cognitive decline, exemplifying the potential of TIM-3 as a therapeutic target in Alzheimer’s treatment strategies.
Current research, including studies conducted on genetically modified mice, shows promising results when TIM-3 inhibition is achieved. By genetically deleting the TIM-3 gene, researchers have observed that microglia regain their ability to actively clear amyloid plaques, leading to improved cognitive functions in these animals. This insight opens new avenues for developing TIM-3 Alzheimer’s treatments, such as anti-TIM-3 antibodies or small molecules that can prevent its inhibitory action, potentially reversing some aspects of cognitive impairment associated with Alzheimer’s disease.
This research emphasizes the need for a deeper understanding of the immune response in the brain and how these mechanisms could be exploited to improve patient outcomes. As Alzheimer’s disease affects millions, exploring strategies that target immune modulation through TIM-3 could provide a new perspective in developing effective Alzheimer’s treatment options.
As studies continue, it is crucial to consider how these findings can be translated into clinical trials. The recent successes in trials employing immune system therapies for other diseases highlight the potential effectiveness of a similar approach for Alzheimer’s. Therefore, the TIM-3 pathway not only contributes to the disease process but also offers a viable target for innovative therapeutic strategies that aim to enhance cognitive improvement in Alzheimer’s patients.
Microglia Function and its Impact on Alzheimer’s Disease
Microglia serve as the brain’s primary immune defense, being responsible for maintaining homeostasis and ensuring the health of neural circuits. Their primary functions include phagocytosis of cellular debris, regulation of synaptic pruning, and facilitation of neural communication. In healthy adults, microglia exhibit a dynamic response to brain activity, providing support for developing synapses and maintaining memory. However, in Alzheimer’s disease, the functionality of microglia becomes compromised due to the upregulation of checkpoint molecules such as TIM-3, obstructing their ability to clear harmful amyloid-beta plaques.
The implications of impaired microglial function in Alzheimer’s disease are profound. With the accumulation of plaques, not only does cognitive decline occur, but the overall health of the brain deteriorates as microglia fail to perform their protective roles. The research that focuses on reversing this impairment, particularly through the deletion of TIM-3, suggests that restoring microglial activity could be essential for developing therapies aimed at combating Alzheimer’s. By ensuring that microglia remain active and capable of clearing plaques, we may improve cognitive functions and overall patient quality of life.
Understanding microglial function in the context of Alzheimer’s expands the framework for potential treatments. By exploring drugs and therapies that can help reactivate these important cells, researchers aim not only to halt disease progression but also to initiate repair processes that restore cognitive function. This holistic approach could transform how we view and treat Alzheimer’s, moving away from just addressing symptoms to a more proactive restoration of brain health.
As we advance in neuroimmunology, the interplay between microglia and Alzheimer’s pathology will continue to be a focal point in research. Future clinical approaches will likely harness this understanding, utilizing strategies that not only target plaque removal but also optimize the immune functionality of microglia to enhance cognitive resilience in patients.
The Potential of Immune System Therapy in Alzheimer’s
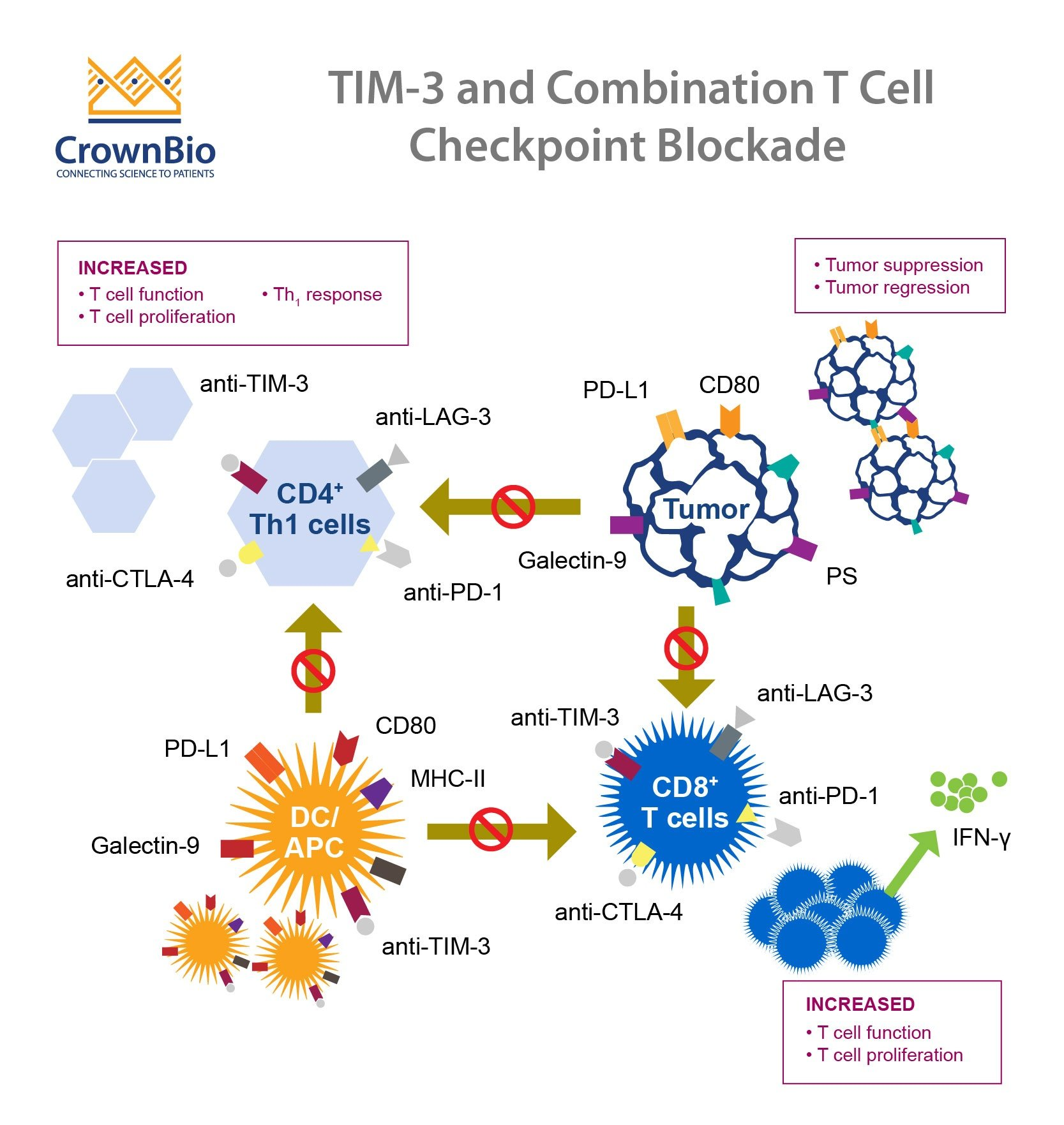
Recent advancements in immune system therapies, especially those inspired by successes in cancer treatment, are now being closely examined for their potential in Alzheimer’s disease management. These therapies often focus on modulating immune responses through the regulation of checkpoint molecules, like TIM-3. The idea is to re-educate the immune system, allowing it to recognize and eliminate pathological structures associated with Alzheimer’s, such as amyloid plaques and tau tangles.
This immunotherapy paradigm represents an exciting frontier in Alzheimer’s research. By utilizing anti-TIM-3 antibodies, researchers can inhibit the negative regulatory effects of TIM-3 on microglia, thereby enhancing their plaque-clearing functions. Since amyloid-beta has also been linked with vascular issues in Alzheimer’s, such therapies could pave the way for improved cognitive outcomes while minimizing risks associated with conventional approaches that often result in vascular damage.
Such innovative approaches not only highlight the importance of immune modulation in the context of Alzheimer’s disease but also raise questions about the future of treatment strategies. The potential to employ immune system therapy as a cornerstone for managing cognitive decline alongside traditional pharmacological interventions could redefine the therapeutic landscape for Alzheimer’s, leading to more effective, combination-based strategies that target various aspects of the disease.
As the research evolves, collaboration between neurologists and immunologists will be crucial in advancing these treatment modalities. There is hope that immune system therapies will not just slow down the disease but restore functional capacity in affected patients, enhancing their quality of life and cognitive abilities.
Cognitive Improvement Through TIM-3 Targeting
Cognitive improvement in Alzheimer’s disease is a subject of great interest, particularly as researchers explore how targeting TIM-3 can facilitate this process. Early studies have shown that by blocking TIM-3, microglia can more effectively engage in clearing amyloid plaques, which has a direct impact on cognitive functions such as memory and learning. In laboratory mice genetically modified to lack the TIM-3 gene, evidence shows that they exhibit significant enhancements in cognitive performance compared to their TIM-3 expressing counterparts.
The results illustrate how TIM-3 acts as a brake on the microglial response. By inhibiting this molecule, it’s possible to unleash the natural plaque-clearing capabilities of these immune cells, which in turn leads to a reduction in plaque burden and an enhancement in cognitive abilities. The regenerative potential of restoring appropriate microglial activity hints at a revolutionary approach to treating Alzheimer’s disease and emphasizes the need for continued research into TIM-3 as a therapeutic target. This focus on cognitive improvement aligns with the ultimate goal of Alzheimer’s therapies, which is not merely to prolong life but to enhance the quality of that life by retaining cognitive functions.
Harnessing TIM-3 targeting strategies may lead to transformative outcomes in Alzheimer’s treatment protocols. Therapies utilizing this approach could allow clinicians to shift from traditional symptomatic treatments to potentially disease-modifying interventions that address the very mechanics of plaque accumulation. Ultimately, the potential for cognitive improvement through TIM-3 modulation represents a hopeful avenue for advancing Alzheimer’s disease management.
As research continues to unfold, the integration of TIM-3 targeting strategies into clinical practice will be of paramount importance. By focusing on restoring cognitive functions alongside managing plaques, we begin to envision a future where Alzheimer’s treatment encompasses holistic brain health restoration, enabling patients to regain lost memories and cognitive clarity.
The Relationship Between Immune System and Alzheimer’s Pathology
The relationship between the immune system and Alzheimer’s disease is becoming increasingly evident, particularly through the lens of TIM-3 and microglial activity. The immune system, traditionally viewed as a defender against pathogens, also plays a dual role in maintaining brain health and responding to pathological changes. In the case of Alzheimer’s, the accumulation of neurotoxic amyloid plaques triggers an immune response that could either mitigate or exacerbate the disease. TIM-3 has been identified as a critical checkpoint molecule that modulates this immune response.
While microglia are designed to clean up debris and respond to injury through phagocytosis, TIM-3 inhibits their effectiveness when activated against amyloid plaques. As a result, the microglial response becomes dysfunctional, leading to an inadequate removal of these harmful structures. This connection to immune function highlights the significance of TIM-3 modulation, presenting it as a target for therapeutic intervention in Alzheimer’s disease. By understanding and manipulating this relationship, researchers can aim for a more robust immune response that not only addresses plaque accumulation but also promotes overall brain health.
This interplay between the immune responses in the progression of Alzheimer’s disease opens up avenues for novel therapeutics targeting immune checkpoints. The concept of immune therapy, particularly immune checkpoint inhibitors, may offer new hope for patients struggling with cognitive decline. By reactivating the immune system’s ability to react appropriately to Alzheimer’s pathology, we can potentially not only halt the progression of cognitive impairment but also restore some aspects of cognitive function that patients have lost.
As new clinical trials and studies emerge, the challenge remains to balance immune activation without inducing excessive inflammation, which can itself be damaging. This dynamic, complex interplay underscores the need for a nuanced approach in developing therapies that contribute to long-lasting cognitive improvements while effectively managing the underlying pathology of Alzheimer’s disease.
Future Directions in Alzheimer’s Research and Treatment
The future of Alzheimer’s research is bright, especially with the discoveries surrounding TIM-3 and its role in immune modulation. As we move forward, the integration of findings from this research into practical treatment options will be critical. The re-purposing of existing anti-TIM-3 antibodies for Alzheimer’s treatment exemplifies a forward-thinking strategy that capitalizes on prior advancements in cancer therapies. This re-evaluation of treatment methodologies signals a possible paradigm shift, aiming to address the root causes of cognitive decline rather than merely managing the symptoms.
Additionally, ongoing collaborations between immunologists and neurologists are essential for synthesizing the knowledge needed to develop innovative therapeutic approaches. Research indicates that successful intervention must focus not only on plaque removal but also on restoring a balanced immune environment in the brain. Such dual-targeted approaches could significantly enhance the efficacy of Alzheimer’s treatments, leading to more sustained cognitive improvements.
The road ahead will involve rigorous testing through clinical trials to validate the efficacy and safety of TIM-3 targeting therapies in human subjects. As patient populations with Alzheimer’s continue to grow, it is crucial to expedite these studies while ensuring high standards of scientific integrity. Emphasizing patient-centric outcomes, future research must strive for therapies that not only slow cognitive decline but actively promote recovery and maintenance of cognitive functions.
Ultimately, the successful development of TIM-3 targeted therapies combined with a comprehensive understanding of Alzheimer’s pathology may transform the treatment landscape for this debilitating disease. By addressing both the biological mechanisms of the disease and the patient’s quality of life, we can aspire to improve health outcomes for those affected by Alzheimer’s in the coming years.
Frequently Asked Questions
What is TIM-3 in the context of Alzheimer’s treatment?
TIM-3 is an immune checkpoint molecule that inhibits the immune system’s response, particularly affecting microglia, the brain’s immune cells. Recent research suggests that targeting TIM-3 may enhance microglial functionality, enabling them to clear amyloid plaques associated with Alzheimer’s disease, thus potentially improving cognitive function.
How does TIM-3 impact microglia function in Alzheimer’s disease?
In Alzheimer’s disease, TIM-3 expression on microglia prevents these cells from attacking and clearing amyloid plaques. By inhibiting TIM-3, researchers aim to reactivate microglia to restore their plaque-clearing ability, which could lead to cognitive improvement in Alzheimer’s patients.
Can TIM-3 therapies improve cognitive function in Alzheimer’s patients?
Emerging studies indicate that therapies targeting TIM-3 may improve cognitive function in Alzheimer’s individuals by enhancing microglial activity against plaques. Animal models show that deleting the TIM-3 gene leads to plaque clearance and improved memory performance.
What role does TIM-3 play as a genetic risk factor for Alzheimer’s disease?
TIM-3 has been identified as a genetic risk factor for late-onset Alzheimer’s disease. Individuals with certain polymorphisms in the TIM-3 gene (HAVCR2) exhibit higher levels of this molecule, which correlates with increased plaque accumulation in the brain, leading to cognitive decline.
How does TIM-3 relate to immune system therapy approaches for Alzheimer’s?
TIM-3, traditionally known for its role in cancer treatment as an immune checkpoint, is being studied for its potential use in Alzheimer’s therapy. By blocking TIM-3, researchers aim to enhance the immune response against Alzheimer’s plaques, paralleling strategies employed in cancer treatment.
What potential strategies utilize TIM-3 for Alzheimer’s disease treatment?
Potential strategies include the use of anti-TIM-3 antibodies or small molecules to inhibit TIM-3’s function, thereby allowing microglia to effectively clear amyloid plaques and restore cognitive functions affected by Alzheimer’s disease.
How long has the research on TIM-3 and Alzheimer’s treatment been ongoing?
Research into TIM-3’s role in Alzheimer’s treatment has spanned five years, with numerous experiments aimed at understanding how TIM-3 impacts microglial function and its potential to reduce plaque burden in models of the disease.
What are the next steps in TIM-3 Alzheimer’s treatment research?
The next steps involve testing human anti-TIM-3 antibodies in mouse models that replicate Alzheimer’s disease pathology. Researchers aim to determine if these antibodies can halt plaque development and improve cognitive outcomes.
| Key Point | Details |
|---|---|
| Research Focus | The study explores the potential of using checkpoint molecules, particularly TIM-3, in treating Alzheimer’s disease. |
| Study Significance | It shows that deleting TIM-3 enhances microglial function to clear amyloid plaques, thereby improving memory in mouse models. |
| Research Collaboration | Conducted by Vijay Kuchroo and Oleg Butovsky, highlighting multidisciplinary collaboration in addressing Alzheimer’s. |
| Implications for Treatment | Potential development of anti-TIM-3 antibodies as a therapeutic approach for Alzheimer’s. |
| Future Directions | Plans to test human anti-TIM-3 for halting plaque development in Alzheimer’s disease mouse models. |
Summary
TIM-3 Alzheimer’s treatment shows promise as new research indicates that targeting the TIM-3 checkpoint molecule may enhance the immune response in the brain to combat the harmful plaques associated with Alzheimer’s disease. By inhibiting TIM-3, researchers have effectively improved memory and cognitive function in mice, encouraging new avenues for therapeutic intervention. Collaboration between experts has paved the way for innovative approaches that could potentially translate into clinical settings, providing hope for improved treatment strategies for Alzheimer’s in the future.