Fighting Alzheimer’s disease is an urgent priority for scientists as millions of Americans grapple with the devastating effects of this neurodegenerative disease. Recent advancements in neuroscience research have revealed groundbreaking truths about microglial cells, which act as the brain’s immune system. According to renowned neuroscientist Beth Stevens, these cells are key players not just in maintaining brain health, but in the formation of Alzheimer’s treatment approaches. By investigating how abnormal microglial activity contributes to synaptic pruning, Stevens has opened doors to early detection and new therapeutic strategies. As the aging population continues to grow, understanding these cellular mechanisms becomes essential for combating the rising tide of Alzheimer’s.
Addressing the challenges of Alzheimer’s, a debilitating condition that affects cognitive function and memory, has never been more critical. Considered one of the leading causes of dementia, this condition is increasingly linked to various neurobiological factors, including the role of immune cells in the brain, known as microglia. The work of innovative researchers like Beth Stevens, who focuses on these crucial cells, sheds light on the underlying mechanisms of this complex disease. Their discoveries pave the way for new diagnostic tools and therapies, offering hope to those affected by this widespread health issue. As the landscape of Alzheimer’s research evolves, understanding these neuroimmune interactions will undoubtedly redefine our approaches to treatment and care.
Understanding Microglial Cells in Alzheimer’s Disease
Microglial cells are crucial components of the brain’s immune system, playing a vital role in maintaining neural health. These cells patrol the brain and are responsible for identifying and clearing out dead or damaged neurons, while also pruning connections between synapses—a critical process for normal brain function. However, recent discoveries by researchers like Beth Stevens reveal that an imbalance in microglial activity can significantly contribute to neurodegenerative diseases such as Alzheimer’s. This aberrant pruning, where microglia become hyperactive or dysfunctional, can lead to synaptic loss and cognitive decline, underscoring the importance of these cells in the pathology of Alzheimer’s.
In the realm of neuroscience research, understanding the behavior of microglial cells offers new avenues for Alzheimer’s treatment. By targeting the mechanisms that regulate microglial pruning, scientists can develop therapeutic strategies that not only halt the progression of Alzheimer’s but also promote neuroprotection and recovery. The Stevens Lab’s groundbreaking work exemplifies how exploring the fundamental biology of these immune cells can pave the way for innovative treatments and early detection biomarkers for Alzheimer’s and other related neurodegenerative disorders.
The Impact of Behavioral Science on Alzheimer’s Research
The transformation in thinking about behavioral science can significantly influence the understanding and treatment of Alzheimer’s disease. Research conducted by leading neuroscientists reveals the interplay between environmental factors and microglial function in the brain. For instance, factors such as diet, exercise, and social engagement can modulate the activity of microglial cells, potentially reducing the risk of neurodegenerative diseases. By incorporating behavioral science insights, researchers like Beth Stevens can design interventions that not only target biological mechanisms but also encourage lifestyle changes that bolster brain health.
Furthermore, studying behavioral patterns among individuals with Alzheimer’s allows researchers to elucidate the progression of cognitive decline. These observations can inform the development of personalized treatment approaches that account for individual lifestyle factors and psychological health. This integrative approach not only enhances our understanding of microglial dysfunction in Alzheimer’s but also advocates for comprehensive care strategies that support patients’ overall well-being, thus playing a critical role in combating this devastating disease.
Innovations in Neurodegenerative Disease Treatments
Innovations in the treatment of neurodegenerative diseases have gained momentum due to advancements in understanding the underlying mechanisms of diseases like Alzheimer’s. The groundbreaking discoveries made by researchers, particularly in the context of microglial cells, have opened potential therapeutic pathways that were previously unforeseen. With insights into how these immune cells operate in the brain, scientists can explore targeted treatment options that aim to restore normal microglial function, potentially reversing the damage seen in neurodegenerative conditions.
Moreover, the collaboration between various research institutions, such as the Stevens Lab at Boston Children’s Hospital and the Broad Institute, emphasizes the importance of interdisciplinary approaches in developing effective Alzheimer’s treatments. By combining basic science with clinical applications, researchers can create a pipeline for translating groundbreaking discoveries into viable treatments. This collaborative model fosters innovation, accelerates the pace of scientific discovery, and ultimately enhances the potential for impactful therapies to benefit millions affected by Alzheimer’s and other neurodegenerative diseases.
Beth Stevens: Pioneering Alzheimer’s Research
As a pioneer in Alzheimer’s research, Beth Stevens has substantially shaped the conversation around microglial cells and their role in neurodegenerative diseases. Her dedication to unraveling the complexities of brain immune responses has led to new frameworks for understanding how these cells influence synaptic health. Stevens’ work emphasizes the necessity for curiosity-driven research, which can yield unexpected insights and lead to groundbreaking applications in Alzheimer’s treatment.
Stevens’ contributions, particularly her recognition as a MacArthur “genius,” highlight the critical link between fundamental research and real-world applications. By advancing our knowledge of microglial functions, her research is instrumental in developing potential biomarkers for earlier diagnosis and intervention in Alzheimer’s disease. This approach could significantly enhance the quality of care for individuals at risk and ensure timely access to treatment, ultimately improving outcomes for those living with Alzheimer’s.
The Role of Federal Funding in Alzheimer’s Discovery
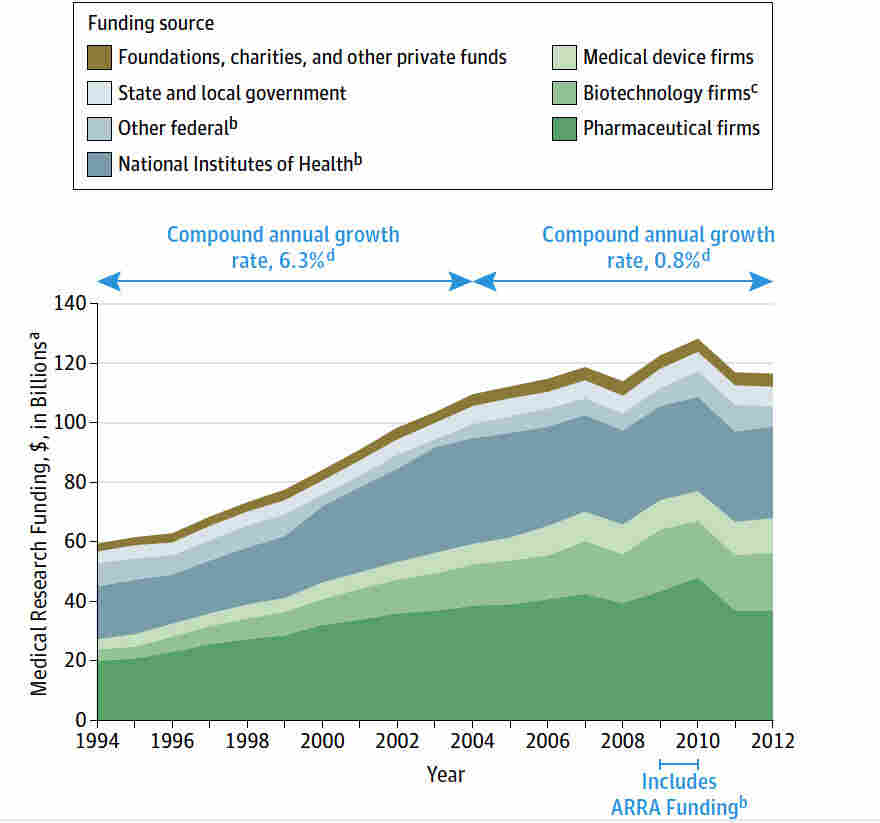
Federal funding plays an essential role in the pursuit of breakthroughs in Alzheimer’s research. Support from agencies like the National Institutes of Health (NIH) not only provides financial resources but also fosters an environment of collaboration among scientists. This funding is crucial for enabling researchers, like Beth Stevens, to pursue innovative projects that may not have immediate commercial viability but are significant for advancing our understanding of neurodegenerative diseases and microglial cell function.
Moreover, federal investments in basic science allow researchers to explore novel theories and concepts, leading to transformative discoveries that lay the groundwork for future therapeutic strategies. For Alzheimer’s, this means a greater potential for developing new treatments that can alleviate the burden of cognitive decline and enhance the quality of life for millions. The ongoing commitment to funding neuroscience research is vital for sustaining progress in the fight against Alzheimer’s and related diseases.
Future Directions in Alzheimer’s Treatment Strategies
Looking ahead, the future of Alzheimer’s treatment strategies is poised to benefit considerably from the ongoing research into microglial cells and their role in the disease’s pathology. As scientists like Beth Stevens continue to uncover the biological mechanisms behind aberrant neural pruning, the development of targeted therapies that modulate microglial activity is becoming increasingly feasible. This represents a shift from traditional symptomatic treatments towards more disease-modifying approaches that address the root causes of Alzheimer’s.
In addition to pharmacological interventions, there is a growing interest in lifestyle modifications that can support brain health and potentially prevent Alzheimer’s. Studies suggest that a holistic approach that incorporates diet, exercise, and cognitive engagement may influence microglial function and promote resilience against neurodegenerative processes. Integrating these strategies into treatment plans not only enhances patient care but also aligns with the broader goal of reducing the incidence of Alzheimer’s within aging populations.
The Importance of Early Detection in Alzheimer’s Disease
Early detection of Alzheimer’s disease is critical for implementing effective treatment strategies and improving patient outcomes. As highlighted by the research conducted in the Stevens Lab, the identification of new biomarkers linked to microglial activity could transform the landscape of Alzheimer’s diagnosis. By detecting the disease process in its initial stages, healthcare providers can offer timely interventions that potentially slow the disease’s progression and enhance cognitive function.
Moreover, the focus on early detection paves the way for preventative measures that can be adopted long before symptoms manifest. Educating individuals about risk factors and encouraging regular cognitive health assessments are vital in building awareness and promoting proactive health behaviors. As the understanding of Alzheimer’s deepens, the drive towards innovation in early detection methods will play a pivotal role in shaping the future of Alzheimer’s care.
Community Engagement in Alzheimer’s Awareness
Community engagement is fundamental in raising awareness and understanding of Alzheimer’s disease. Initiatives that foster public dialogue around the disease can demystify Alzheimer’s and mobilize support for research efforts. Through community education programs, individuals can learn about the importance of microglial cells in brain health, the risks of neurodegenerative diseases, and how scientific advancements can translate into improved treatment options. Beth Stevens’ innovative research underscores the necessity for such discussions, as increasing public awareness can directly influence funding and policy decisions in Alzheimer’s research.
Furthermore, engaging communities facilitates connections among researchers, patients, and caregivers, creating a support network that empowers those affected by Alzheimer’s. Community-led forums can encourage shared experiences and foster a collaborative approach to addressing the challenges posed by the disease. This interconnectedness is essential not only for advancing scientific research but also for building a compassionate society that understands and supports individuals living with Alzheimer’s.
How Basic Science Fuels Alzheimer’s Breakthroughs
Basic scientific research serves as the foundation for breakthroughs in Alzheimer’s disease treatment. The ongoing exploration of fundamental biological processes, such as the functions of microglial cells, reveals insights that are critical for developing effective therapeutic strategies. Researchers like Beth Stevens exemplify how passion for basic science can lead to unexpected discoveries, such as the impact of microglial pruning on synaptic health and overall brain function.
Without the groundwork laid by curiosity-driven research, advancements in Alzheimer’s treatment would stall. The Stevens Lab’s commitment to understanding the intricate roles of the brain’s immune system demonstrates how basic research translates into real-world applications for Alzheimer’s care. As new findings emerge, they pave the way for innovative therapies that directly improve the lives of those living with this complex disease.
Frequently Asked Questions
How do microglial cells contribute to fighting Alzheimer’s disease?
Microglial cells play a crucial role in fighting Alzheimer’s disease as they function as the brain’s immune system. They patrol for signs of illness and injury, clear out dead cells, and prune synapses that transmit information among neurons. However, aberrant pruning by microglia can contribute to neurodegenerative diseases like Alzheimer’s, highlighting the need for research to better understand and harness their functions.
What breakthroughs have been made in neuroscience research regarding Alzheimer’s treatment?
Recent neuroscience research led by scientists like Beth Stevens has uncovered important insights into the role of microglial cells in Alzheimer’s disease. Her lab’s findings indicate that improper pruning of synapses by microglia may exacerbate the disease, paving the way for new treatments and biomarkers that could detect Alzheimer’s earlier, enhancing intervention strategies.
What is the relationship between neurodegenerative disease and microglial cell function?
Neurodegenerative diseases, such as Alzheimer’s, may be closely linked to the dysfunction of microglial cells. These cells are responsible for maintaining brain health by clearing damaged cells and supporting neuronal connections. When microglial activation and pruning become aberrant, it can result in the progression of neurodegenerative diseases, emphasizing the need to study these cells for effective treatments against Alzheimer’s.
How might Beth Stevens’ research impact future Alzheimer’s treatments?
Beth Stevens’ research has significant implications for future Alzheimer’s treatments. By understanding how microglial cells function and their role in synaptic pruning, her findings could lead to innovative therapies targeting these immune cells to mitigate the effects of Alzheimer’s disease and other neurodegenerative conditions, ultimately enhancing the quality of life for millions of patients.
Why is basic science important in the fight against Alzheimer’s disease?
Basic science is essential in the fight against Alzheimer’s disease because it lays the foundation for understanding complex biological processes. Research initiatives like those led by Beth Stevens illuminate how microglial cells interact within the brain, which can lead to breakthroughs in diagnosis and treatment methods that translate into real-world applications for combating Alzheimer’s.
What role do biomarkers play in fighting Alzheimer’s disease?
Biomarkers are critical in fighting Alzheimer’s disease as they provide measurable indicators of the disease’s presence and progression. Recent discoveries in neuroscience research aim to establish new biomarkers based on microglial cell activity, which could enable earlier detection and more effective intervention for Alzheimer’s, ultimately improving patient outcomes.
How can understanding microglia shed light on neurodegenerative diseases like Alzheimer’s?
Understanding microglia is pivotal for shedding light on neurodegenerative diseases such as Alzheimer’s because these cells are integral to the brain’s immune response. Research demonstrates that microglial dysfunction can lead to synapse loss and neuroinflammation, key features of Alzheimer’s disease. Insights gained from microglial studies can inform potential therapeutic strategies to combat the disease.
| Key Points |
|---|
| Neuroscientist Beth Stevens studies microglial cells, which act as the brain’s immune system. |
| Microglia are crucial in clearing damaged cells and pruning synapses, but their malfunction can contribute to Alzheimer’s disease. |
| Research from Stevens’ lab leads to the potential for new medicines and earlier detection of neurodegenerative diseases. |
| Increased understanding of microglial function paves the way for improved treatments for approximately 7 million Americans with Alzheimer’s. |
| The cost of Alzheimer’s care could rise from $360 million to $1 trillion by 2050 as the population ages. |
| Stevens emphasizes the importance of basic science and perseverance in driving impactful research. |
Summary
Fighting Alzheimer’s disease involves groundbreaking research into the role of microglial cells, which serve as the brain’s immune defense. By understanding how these cells function and their impact on neurodegenerative conditions, scientists like Beth Stevens are uncovering new pathways to develop effective treatments. As the population ages and the caseload for Alzheimer’s increases, ongoing research is essential in combating this growing health crisis. Through foundational studies and curiosity-driven science, we can foster innovations that enhance the quality of life for millions affected by Alzheimer’s.