CRISPR ethics presents a critical crossroads in the realm of modern medicine, as the powerful gene editing technology has the potential to revolutionize treatments such as sickle cell cures. While the promise of eradicating genetic diseases sparks much hope, it brings forth troubling ethical questions regarding our right to alter human genetics. Discussions around health equity and medical ethics are increasingly pertinent as we navigate the implications of CRISPR technology. Who decides which genes merit alteration, and at what cost? As scientists and ethicists explore these dilemmas, it is essential to consider not only the medical benefits but also the broader societal consequences of gene editing.
Exploring the nuances of CRISPR ethics involves delving into the moral fibers that entwine with advancements in gene modification. This dialogue encompasses discussions about genomic interventions, particularly in contexts like curing hereditary illnesses such as sickle cell anemia. Moreover, the intersection of health equity with these medical innovations raises pressing concerns about accessibility and just distribution of cutting-edge treatments. As we ponder the implications of bioethical principles in the application of CRISPR technology, we must critically evaluate the responsibilities we hold in shaping the genetic future of humanity. Ultimately, as we push the boundaries of what is possible in gene editing, we are compelled to confront the philosophical considerations that accompany our scientific ambitions.
The Promise of Gene Editing: A New Era in Medicine
Gene editing technology, particularly CRISPR, heralds a transformative era in medicine, offering the potential to address genetic disorders and diseases that have long plagued humanity. With advancements such as the ability to modify somatic and germline cells, scientists can effectively eliminate the genes responsible for conditions like sickle cell disease. This capability not only provides a pathway to curing patients but also highlights the innovative applications of gene editing in modern medicine. As healthcare continues to evolve, the use of CRISPR technology stands at the forefront, promising unprecedented solutions to age-old health challenges.
However, the excitement surrounding gene editing is tempered by significant ethical considerations. The implications of altering genetic material pose deep questions about what constitutes a ‘normal’ human condition. While curing life-threatening diseases is universally embraced, the application of CRISPR to traits that are not pathologies, such as height or intelligence, raises ethical dilemmas about parental choice and societal impact. The crux of the debate lies in balancing the potential benefits of gene editing against the moral responsibility we hold to maintain the essence of human diversity.
Health Equity in Gene Editing: Addressing Disparities
As CRISPR technology advances, the issue of health equity becomes increasingly critical. The high cost of gene editing therapies, such as a sickle cell cure priced at approximately $2.2 million, raises urgent questions about access and affordability. If such groundbreaking treatments are only available to a wealthy minority, the potential to widen existing health disparities becomes a stark reality. This situation demands a conscious effort from policymakers, healthcare providers, and society at large to ensure that the benefits of gene editing do not become privileges reserved for the affluent, but are equitably accessible to all.
Furthermore, with an estimated 100,000 individuals in the U.S. suffering from sickle cell, global health equity becomes an even greater concern. The disparity in access to healthcare technologies between developed and developing nations illustrates a significant gap. As emphasized during discussions surrounding the ethics of gene editing, equity in healthcare is not just a matter of fairness; it is a fundamental aspect of public health. We must explore innovative financing models and governmental strategies to democratize access to potentially life-saving gene therapies, ensuring that progress in medical science truly benefits everyone.
Medical Ethics and Gene Editing: Navigating Complex Dilemmas
The rapid advancement of CRISPR technology brings with it a series of complex medical ethics questions that require careful navigation. As discussed by experts like Neal Baer and Rebecca Brendel, the stakes involved in editing genes extend beyond the biological to encompass profound ethical implications. For instance, when considering whether to modify embryos or treat conditions that are not life-threatening, such as Down syndrome, we must ask who has the authority to make these critical decisions. The balance of power in determining the nature of human health and variation raises pivotal ethical concerns about autonomy, consent, and societal norms.
Moreover, the potential for unintended consequences from gene editing compounds the ethical quandaries faced by medical professionals and researchers. The intricacies of genetic interactions mean that changing one gene could have unforeseen effects on a myriad of other biological processes. As advancements in medical science pave the way for CRISPR applications, the ethical responsibility of researchers to thoroughly understand and communicate these risks is paramount. The conversation must not only center around the ‘can we’ but also delve deeply into the ‘should we,’ ensuring that our scientific pursuits align with ethical standards of care and respect for human diversity.
CRISPR Ethics: Balancing Innovation and Responsibility
The ethics surrounding CRISPR technology have ignited fervent debate in both the scientific community and society at large. As advancements in gene editing capabilities continue to evolve, the question of whether we ought to pursue certain modifications is a central theme of ethical discourse. The potential to design traits or eliminate genetic conditions poses significant philosophical dilemmas: Should we intervene in nature, and if so, to what extent? Experts like Neal Baer caution against hasty applications of this powerful tool, emphasizing the need for thorough ethical considerations before implementation.
Furthermore, oversight remains a pivotal component in the conversation about CRISPR ethics. The current regulatory framework struggles to keep pace with rapid scientific advancements, leaving room for potential misuse or irresponsible experimentation. Calls for a robust ethical framework to govern gene editing practices are growing louder as the implications of CRISPR extend beyond individual patients to society at large. The challenge lies in establishing guidelines that prioritize humanity’s shared values while fostering innovation in health technologies, ensuring that ethical standards do not stifle scientific progress but instead guide it toward socially responsible outcomes.
The Role of Society in Shaping Gene Editing Policies
As society stands on the brink of unprecedented gene editing capabilities, the role of public discourse and social values in shaping policies cannot be understated. Engaging diverse voices in discussions about the implications of CRISPR technology—including ethicists, healthcare professionals, patients, and the broader public—is crucial for transparent and informed decision-making. Given that gene editing will likely impact future generations, societal input is necessary to navigate the ethical landscape and establish norms that are congruent with our collective values.
Moreover, educational initiatives that inform and involve the public in gene editing discussions can drive more equitable and ethical uses of this technology. Raising awareness about the potential benefits and risks associated with gene editing, as well as the importance of health equity, can help foster a more informed electorate that advocates for policies aligning with ethical standards. As policymakers shape regulations, societal involvement ensures that the voices of those affected by gene editing—particularly marginalized communities—are heard and considered in the unfolding narrative of health innovations.
Assessing the Impact of Gene Editing on Future Generations
The long-term implications of gene editing using CRISPR technology on future generations pose significant questions for researchers and ethicists alike. When alterations are made to germline cells, the changes are heritable, meaning they will affect not just the individual but their descendants as well. This permanence necessitates a cautious approach, as the consequences of these genetic modifications may unfold over decades. Discussions about the ethical limits of gene editing must consider the potential societal ramifications of introducing heritable modifications that may alter human evolution itself.
Furthermore, as we contemplate the potential for ‘designer babies’ or the engineered traits that may emerge from gene editing, we must ask ourselves what kind of future we wish to create. Will these technologies serve to enhance human experience, or will they narrow the diversity that constitutes our humanity? Ethical foresight is crucial in determining how we navigate the intersection of science, culture, and human dignity as we explore the transformative potential of gene editing for the generations to come.
Gene Editing in the Contemporary Medical Landscape
The contemporary medical landscape is increasingly shaped by the advent of gene editing technologies like CRISPR. These tools not only promise novel therapeutic strategies for previously untreatable genetic disorders, but they also challenge existing medical paradigms. Treatments for diseases such as sickle cell anemia are just the beginning; as scientists unravel the complexities of human genetics, the range of conditions that could potentially be treated via gene editing expands. This innovation is driving a new age of personalized medicine, where therapies are tailored to the individual genetic profile of each patient.
However, as gene editing gains traction within the healthcare system, it is imperative to confront the associated ethical dilemmas. The integration of gene editing into clinical practice raises critical questions about patient consent, access to technology, and the potential for inequity in treatment options. As researchers and healthcare providers embrace the power of CRISPR, they must also commit to upholding ethical standards that prioritize patient welfare and equitable access to cutting-edge treatments, ensuring that the benefits of gene editing extend to all segments of society.
Navigating the Technical Challenges of Gene Editing
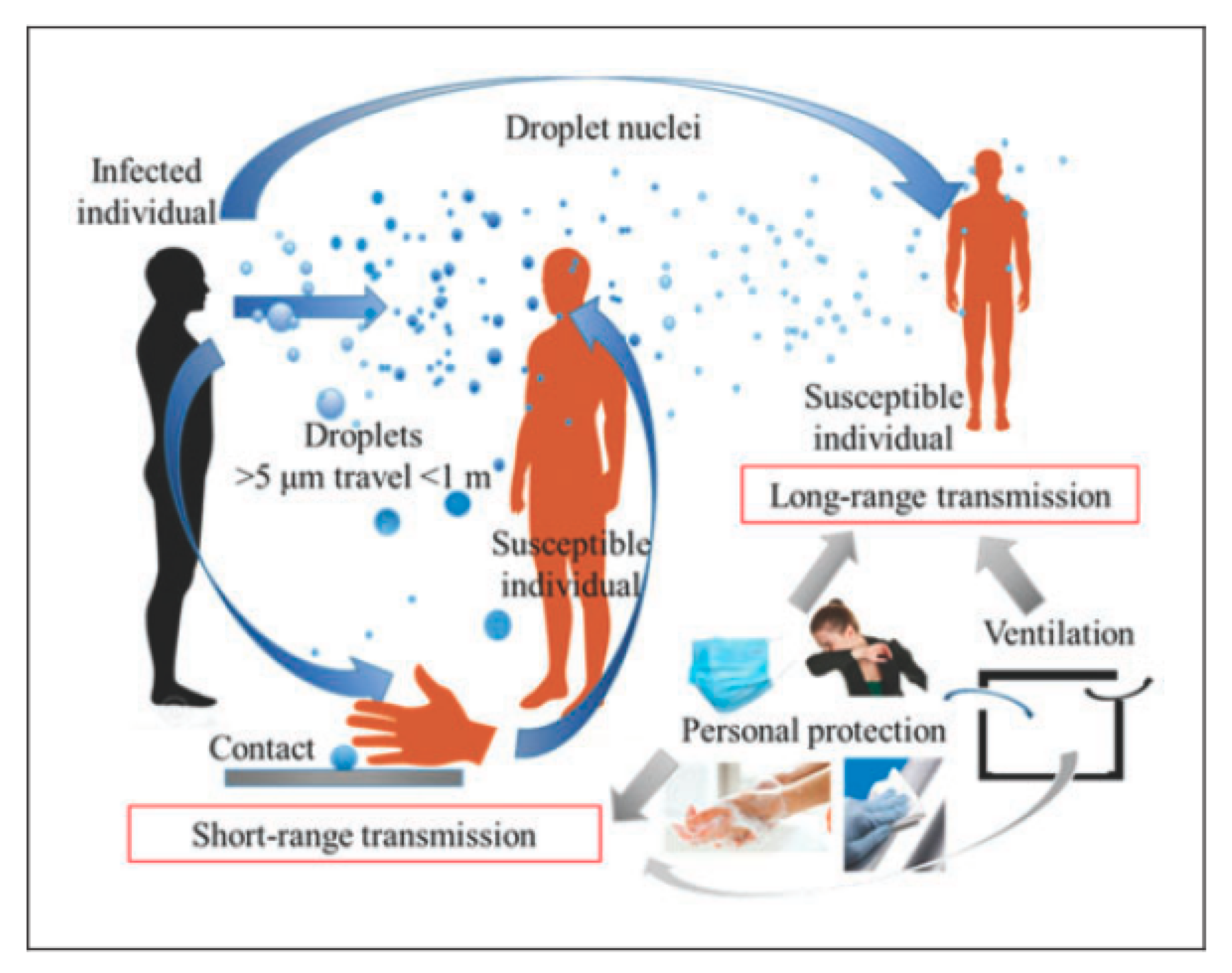
Though gene editing using CRISPR holds immense promise, it is not without its technical challenges. The precision required in altering specific genes is a leading concern among scientists and researchers. Off-target effects, where unintended modifications occur in the genome, can lead to unforeseen consequences that may pose serious health risks to patients. Ongoing research is focused on improving the accuracy of gene editing techniques to minimize these risks and enhance the safety profile, which is paramount as these technologies transition from the bench to the bedside.
Additionally, the delivery mechanism of CRISPR components into the target cells presents its own set of hurdles. Achieving efficient and effective delivery remains a cornerstone of successful gene editing applications. Various methods, including viral vectors and lipid nanoparticles, are being explored to enhance delivery efficacy. Addressing these technical challenges is crucial for realizing the full therapeutic potential of gene editing, ensuring that CRISPR technology can be safely and effectively used in treating diseases while minimizing any risks associated with its application.
Future Directions: The Evolving Role of CRISPR in Healthcare
As CRISPR technology continues to evolve, its role in healthcare is poised to expand significantly over the coming years. The potential applications of gene editing are vast, ranging from the treatment of genetic disorders to applications in regenerative medicine and beyond. By harnessing the power of CRISPR, researchers are exploring innovative avenues to alter the course of diseases, improve tissue repair, and even combat complex conditions like cancer. The pace of discovery in this field suggests that we are merely scratching the surface of what is possible.
However, this rapid advancement also underscores the need for a robust ethical framework and regulatory oversight as CRISPR technologies become integrated into clinical practices. The challenges of ensuring equitable access, managing risk, and maintaining ethical standards in gene editing will necessitate widespread collaboration among scientists, ethicists, healthcare practitioners, and policymakers. As we stand on the brink of a new era in medicine, it is crucial to steer the future directions of CRISPR in a way that prioritizes both scientific innovation and the ethical implications of transforming human health.
Frequently Asked Questions
What ethical concerns arise from using CRISPR technology for gene editing?
CRISPR technology raises several ethical concerns related to gene editing, particularly regarding the implications of altering human genetics. These include issues of consent, as future generations cannot consent to germline edits, and the potential for eugenics, where certain traits may be preferred over others. Additionally, the accessibility and cost of CRISPR-based treatments, such as cures for diseases like sickle cell anemia, pose concerns about health equity and whether only wealthy individuals will benefit from these advancements.
How does CRISPR technology propose to cure sickle cell anemia?
CRISPR technology can potentially cure sickle cell anemia by editing the genes responsible for the disease. This involves targeting and modifying somatic cells to remove the defective genes that cause the disorder. If germline editing is pursued, it could prevent the disease from affecting future generations altogether. However, while the prospect of a cure is promising, it raises significant ethical considerations regarding the impacts on individuals and society.
What is the relationship between CRISPR ethics and health equity?
CRISPR ethics directly relates to health equity as the advancements in gene editing may create disparities in access to treatments. As seen with the example of sickle cell cures costing over $2 million, financial barriers could restrict such innovations to affluent populations, exacerbating existing health inequities. Ethicists argue that it’s crucial to ensure that emerging technologies like CRISPR are accessible to all, regardless of socioeconomic status, to promote fairness in healthcare.
What are the implications of CRISPR for diseases that are not life-threatening?
The ethical implications of using CRISPR for non-life-threatening diseases, such as Down syndrome, raise complex questions. Such decisions could lead to a society that values certain traits over others, potentially sidelining individuals with disabilities. This presents a slippery slope regarding parental rights and the definition of what constitutes a ‘healthy’ child. The discussion around this issue emphasizes the need for ethical guidelines and public discourse to navigate these challenging waters.
Why is oversight essential in the application of CRISPR technology?
Oversight is critical in the application of CRISPR technology to prevent misuse and potential unethical applications, such as unauthorized germline editing or genetic manipulation for enhancement purposes. With concerns of countries such as Russia and China not complying with ethical standards, there is a risk of ‘rogue science’ that could lead to unintended consequences. Effective oversight ensures that gene editing is conducted responsibly, prioritizing safety and ethical considerations alongside scientific advancement.
Can altering genetics with CRISPR have unintended consequences?
Yes, altering genetics with CRISPR can lead to unintended consequences due to the complexity of gene interactions. For instance, while editing a gene for lowering LDL cholesterol may seem beneficial, it can affect numerous other biological processes. These unintended effects highlight the necessity for comprehensive research and cautious implementation of CRISPR technology, as changes in the genetic code could have ripple effects throughout an organism’s health.
What are the responsibilities of biomedical professionals in the field of CRISPR ethics?
Biomedical professionals have the responsibility to engage in ethical deliberation regarding CRISPR technology’s use and implications. This includes advocating for equitable access to gene editing therapies, considering the long-term effects of genetic modifications, and emphasizing the importance of informed consent. They must also address societal concerns and actively participate in policymaking to guide the ethical use of CRISPR, ensuring that advancements benefit humanity as a whole.
| Key Points | Details |
|---|---|
| Introduction to CRISPR Ethics | A discussion on the promise and peril of CRISPR gene editing technology, focusing on the ethical questions it raises. |
| The Impact of CRISPR on Health | CRISPR can potentially cure diseases like sickle cell anemia but raises ethical issues about the right to alter human genetics. |
| Cost and Access | The cure for sickle cell costs around $2.2 million, creating concerns about access and equity in healthcare. |
| Ethical Decision-Making | Questions about who decides the appropriateness of gene editing for various conditions, such as Down syndrome. |
| Social and Moral Implications | Concerns that innovation could deepen health inequalities; need for a focus on health justice. |
| Oversight and Regulation | Issues surrounding the global regulation of gene editing practices, with potential for unethical applications. |
| Potential Unintended Consequences | Editing genes can have complex effects as genes interact in ways not fully understood, leading to unforeseen problems. |
Summary
CRISPR ethics is a critical discourse in today’s scientific community, addressing the profound implications of gene editing technologies. As innovations like CRISPR create opportunities to cure diseases, they simultaneously raise urgent ethical questions about the nature of human intervention in genetics. From the implications of altering traits to ensuring equitable access in healthcare, the dialogue surrounding CRISPR is essential for guiding future developments in medicine.