U.S. maternal mortality remains a shocking public health crisis, as the nation leads its high-income peers with an alarming rate of pregnancy-related deaths. This disturbing trend has continued to rise, revealing significant maternal health disparities that are exacerbated by systemic inequalities and inadequate postpartum care. With over 80% of these deaths deemed preventable, there is an urgent call to action for improving healthcare access, particularly for populations affected by chronic conditions like cardiovascular disease during pregnancy. Addressing issues such as these is crucial for reducing maternal mortality rates and ensuring safer pregnancies for all women across diverse racial and ethnic backgrounds. As the U.S. grapples with this ongoing challenge, understanding the holistic needs of mothers can pave the way for transformative public health strategies.
The escalating rates of maternal deaths within the United States are indicative of a broader issue surrounding maternal health. Events related to pregnancy and childbirth are increasingly leading to fatalities, highlighting the need to investigate underlying causes and healthcare access. The disparities observed in maternal outcomes across different demographics demand solutions that include enhanced postpartum support and educational outreach. Factors such as cardiovascular issues emerging during pregnancy underscore the necessity for comprehensive prenatal care. As discussions around reducing maternal fatalities gain momentum, a collective effort is essential to rewrite the narrative surrounding maternal health in America.
Rising Rates of U.S. Maternal Mortality
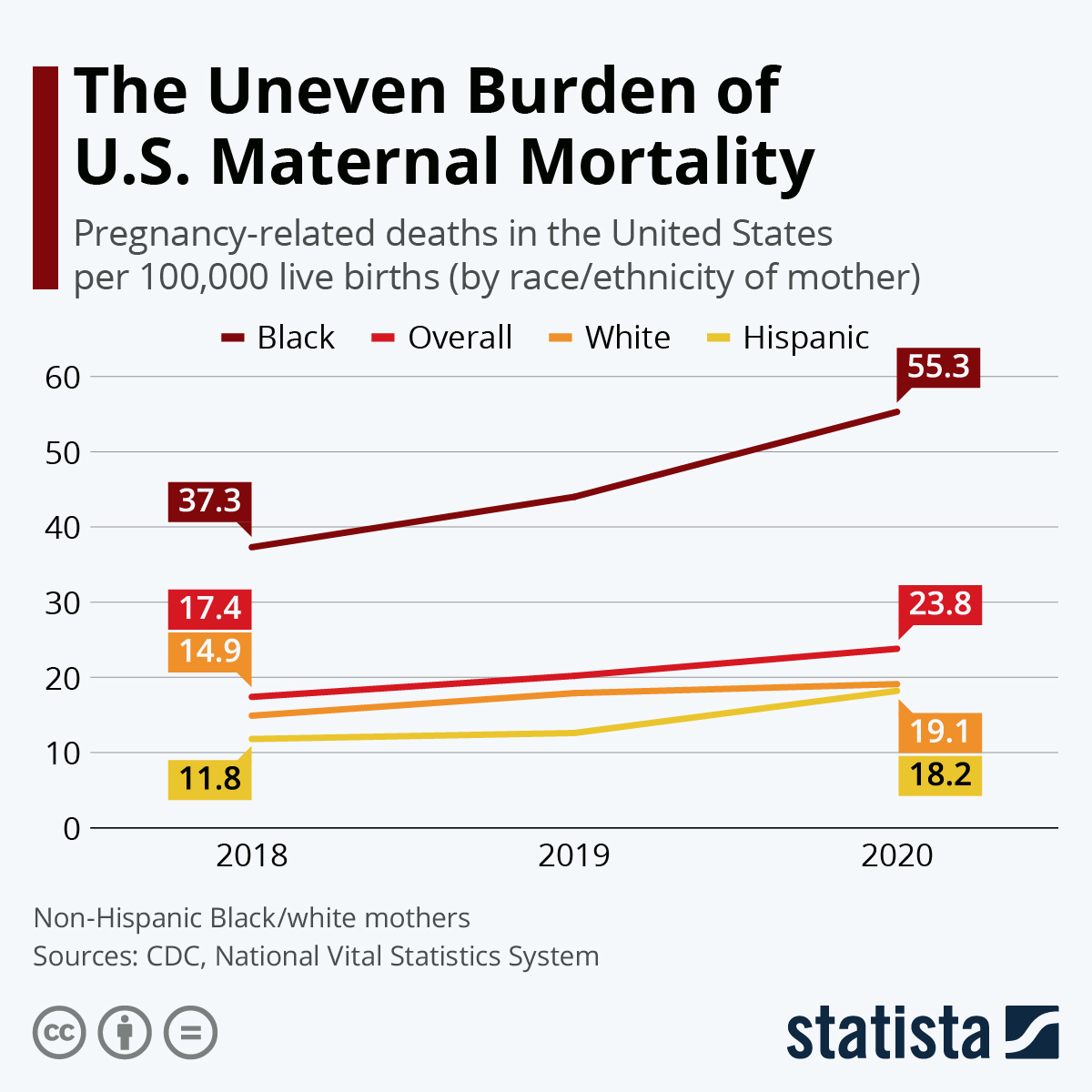
The statistics surrounding maternal mortality in the U.S. are alarming, with the nation leading high-income countries in pregnancy-related deaths. From 2018 to 2022, the maternal mortality rate rose significantly, highlighting the urgent need for improved healthcare strategies. Factors contributing to this crisis include systemic disparities in access to care, particularly among communities of color and lower-income populations. The study revealed that 80% of these deaths are preventable, underscoring the critical importance of addressing root causes such as healthcare inequities, biased treatment practices, and the availability of quality prenatal and postpartum care.
Moreover, racial disparities in maternal mortality rates exemplify the complexities of this public health crisis. For instance, American Indian and Alaska Native women face mortality rates that are nearly four times higher than those of white women, indicating that multifaceted approaches are needed to combat these inequalities. The presence of a healthcare system that inadequately supports marginalized populations contributes to higher risks and complications during pregnancy and the immediate postpartum period. By focusing on these systemic issues, there lies potential in reducing U.S. maternal mortality rates.
Frequently Asked Questions
What are the main reasons behind the rising U.S. maternal mortality rates?
U.S. maternal mortality rates are rising due to a combination of factors including a patchwork healthcare system, inequitable policies, and disparities in access to maternal care. These issues are compounded by the increasing prevalence of chronic medical conditions, such as cardiovascular disease, among pregnant individuals.
How do health disparities impact U.S. pregnancy-related deaths?
Health disparities significantly impact U.S. pregnancy-related deaths, with alarming differences observed among racial and ethnic groups. For instance, American Indian and Alaska Native women face nearly four times the maternal mortality rate compared to white women. Addressing these disparities through targeted policies and inclusive healthcare practices is crucial for reducing maternal mortality.
What role does postpartum care play in reducing U.S. maternal mortality?
Postpartum care is essential for reducing U.S. maternal mortality as nearly one-third of pregnancy-related deaths occur after the initial postpartum period. Expanding healthcare access beyond the immediate weeks post-delivery is vital for managing ongoing health issues and ensuring comprehensive maternal health support.
What is the relationship between cardiovascular disease and pregnancy-related deaths in the U.S.?
Cardiovascular disease has emerged as the leading cause of U.S. pregnancy-related deaths, accounting for over 20% of fatalities. The rise in cardiovascular conditions, such as hypertension and eclampsia, among younger pregnant populations demands heightened awareness and better management during and after pregnancy.
How can states improve their rates of pregnancy-related deaths?
States can improve pregnancy-related death rates by implementing effective policies that focus on equitable healthcare access, enhancing quality of care during pregnancy, and strengthening postpartum support systems. Sharing best practices from states with lower mortality rates, such as California, can guide improvements nationwide.
Why is it important to address late maternal deaths in maternal health discussions?
Addressing late maternal deaths, which occur between 42 days and one year after childbirth, is crucial as they highlight ongoing health risks that new mothers face. Expanding definitions of maternal mortality to include this period underscores the need for continuous healthcare support throughout the postpartum recovery phase.
What steps should be taken to improve public health infrastructure related to maternal health?
Improving public health infrastructure requires increased investment in maternal health research, enhanced training for healthcare providers, and the development of comprehensive policies that address the quality of care during pregnancy and afterward. A focus on equitable access to services can ultimately reduce maternal mortality rates.
What impact did the COVID-19 pandemic have on pregnancy-related deaths in the U.S.?
The COVID-19 pandemic negatively impacted U.S. pregnancy-related deaths, particularly evident in 2021. The pandemic likely exacerbated existing healthcare disparities and created additional challenges in accessing maternal care. Ongoing research is necessary to understand the full spectrum of the pandemic’s effects on maternal mortality.
How do variations in state maternal mortality rates indicate a need for policy changes?
Variations in state maternal mortality rates reveal significant disparities in healthcare access and outcomes. For example, states with lower mortality rates often have better maternal care policies in place. Identifying and emulating these successful strategies can inform national efforts to reduce maternal mortality.
| Key Findings | Statistics | Contributing Factors | Recommended Actions |
|---|---|---|---|
| Maternal mortality rates in the U.S. continue to rise, with significant disparities based on race and geography. | 32.6 deaths per 100,000 live births in 2022 (up from 25.3 in 2018). | Inequitable healthcare systems, chronic medical conditions, and racial discrimination. | Invest in public health infrastructure and innovative care solutions during pregnancy and postpartum. |
| Over 80% of pregnancy-related deaths are preventable; highest mortality rate among high-income countries. | American Indian and Alaska Native women: 106.3 per 100,000; white women: 27.6; non-Hispanic Black women: 76.9. | Maternity care deserts and lack of access to quality care contribute to high rates. | Address policy disparities across states to improve maternal health outcomes. |
| Cardiovascular disease is the leading cause of pregnancy-related death, replacing hemorrhage. | Increase in deaths observed across all age groups since 2018, particularly among 25-39 year-olds. | Chronic conditions like hypertension are emerging at younger ages, posing new risks. | Enhance tracking and reporting systems for maternal deaths, expanding definitions to include late maternal deaths. |
| Late maternal deaths (42 days to one year post-pregnancy) account for nearly a third of total deaths. | COVID-19 pandemic impacts also reflected in rising mortality rates. | Medical bias and discrimination affect care quality and outcomes. | Advocate for better access to comprehensive maternal healthcare, addressing systemic barriers. |
Summary
U.S. maternal mortality remains a pressing issue, with rates that continue to rise above those of other high-income countries. Despite over 80 percent of these deaths being preventable, disparities persist across different racial and ethnic groups. The findings emphasize the urgent need for systemic changes in healthcare practices and policies to address maternal health and create equitable access to care. Addressing the rising trends in pregnancy-related mortality, particularly among marginalized populations, is crucial for improving health outcomes and ensuring safer pregnancies.